Antibiotic Resistance Reduction: probiotics to the rescue, again!
- info848287
- Jul 8, 2025
- 5 min read
Updated: Aug 6, 2025
Antibiotics are life-saving medications, there’s no question about that. The discovery of drugs that could cure pneumonia, prevent infections after surgery, and treat most bacterial infections saved a lot of lives: they were rightly hailed as wonder drugs.
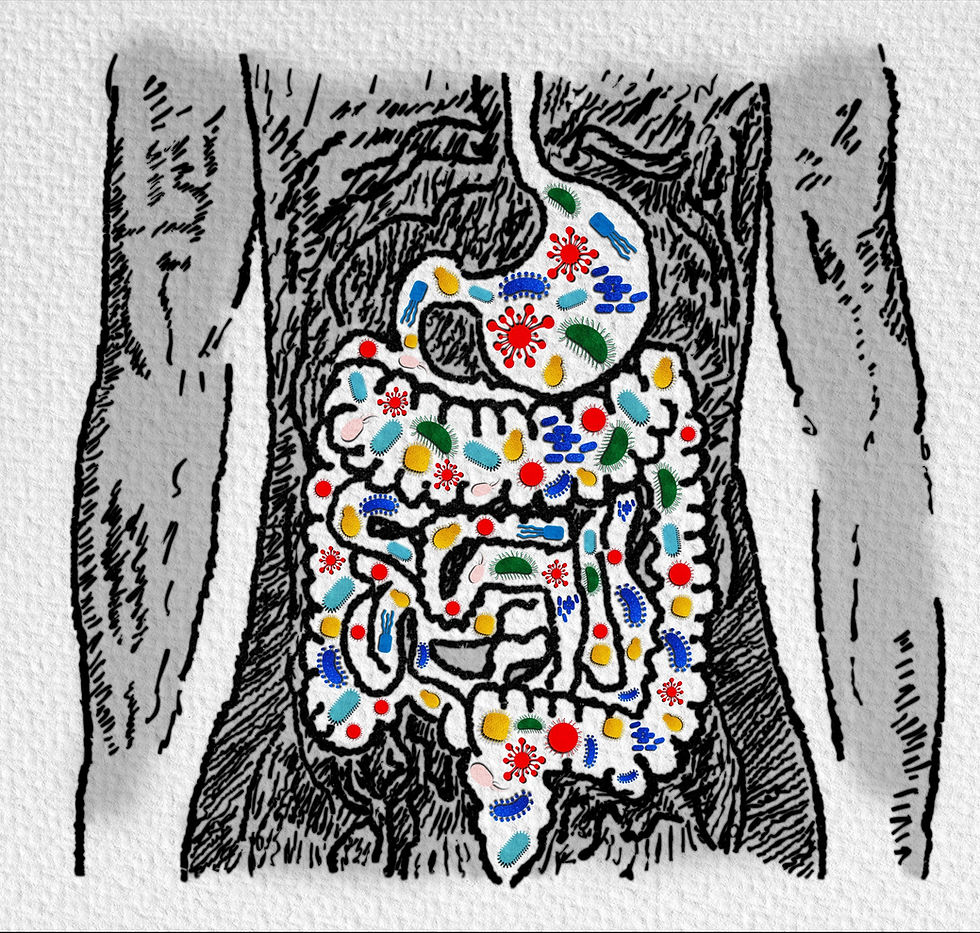
But with big positives we often find some unexpected negatives. We now know that we have at least as many microbes in our gut as there are cells in our bodies, and the majority of them are bacteria. We also know that many of them are killed off by the antibiotics aimed at killing the bad guys: collateral damage associated with adverse side-effects.
Dr. Robert Fleming, who discovered antibiotics, said that we should use them wisely, because overuse could result in them no longer working for us. And time has shown that he was right! It is a pity we didn’t pay more attention to him at the time, before we over-used antibiotics, both as medicines and in farming. Many people still put the antibiotic cream polysporin onto all sorts of skin problems that have nothing to do with bacteria!
Some people experience diarrhea when taking antibiotics. And we have learned that the bad bugs that remain at the end of taking a course of antibiotics are often antibiotic-resistant ones, which is how they have survived despite those antibiotics. But they are the ones that we really don’t want to flourish, precisely because they are antibiotic resistant! In the absence of other helpful bacteria, these get a chance to fill in the gaps created by antibiotic use. So an acute problem has been solved, but a longer-lasting one may have been created.
How can you get the benefits of antibiotics and reduce the harms? Good old probiotics!
People once thought that there wasn’t much point in taking probiotics when you were on a course of antibiotics: you’d just be killing many of them off with the next dose of antibiotics.
But then it was discovered taking probiotics while on a course of antibiotics reduces the diarrhea that can be triggered by the medication. A systematic review published in 2021 concluded that “probiotics are effective for preventing antibiotic-associated diarrhea”. The most helpful ones were of the lactobacillus and bifidobacteria strains.
A serious illness from antibiotic use is caused by the bacterium Clostridium difficile, which can produce a toxin that triggers severe debilitating diarrhoea that can be deadly, especially in the elderly. Probiotics have been shown to reduce the amount of clostridium difficile toxin production, mitigating this problem.
Trials of high-quality probiotics taken between doses of a course of antibiotics, have been shown to reduce the amount of E. coli bacteria resistant to the antibiotic amoxicillin. So providing these when on antibiotic therapy results in fewer antibiotic resistant bacteria left in the gut at the end of the course of treatment. This means fewer bad guys that could then increase in the gut, and which would all, of course, be resistant to those antibiotics. There are just a few trials on a few probiotics, but they all seem to demonstrate the principle that probiotics can help reduce antibiotic resistance. We look forward to seeing more trials on this topic.
Antibiotic resistance is a rising problem in the world, so much so that there is real concern that in the future we may no longer have effective antibiotics to use against bacterial infections. Resistance genes can be passed on to other bacteria, because bacteria share their survival genes with each other. The fewer gut bacteria with those genes, the less likely they are to pass on that capability to other bacteria. Reducing this isn’t just helping you, it’s helping everyone, by slowing the spread of antibiotic resistance.
Also important, it has been found that using probiotics along with antibiotics can help the antibiotics work better. When using antibiotics against Helicobacter pylori (the bacteria associated with stomach ulcers), “Recent studies have shown that probiotic supplementation ….. can enhance the antibiotic effect to achieve a better therapeutic result and maintain the balance of the host gastrointestinal microbiota”. And that “their use associated with standard treatment as an adjunct will improve the eradication rates and decrease treatment-related side effects”. This is especially important as Helicobacter are becoming increasingly resistant to one of the three main antibiotics that are combined to treat them.
In another example, in long-term antibiotic treatment for tuberculosis, where antibiotics are used for many months, probiotics actually reduced the length of antibiotic treatment necessary because, again, the probiotics helped the antibiotics to work better: double bonus!
And there’s more: using probiotics in conjunction with antibiotics reduces the proliferation of the yeast Candida albicans in people’s digestive systems from antibiotic therapy. Increased Candida may cause immediate problems, for example in women who get a vaginal yeast infection after a course of antibiotics. If someone had a fairly high yeast load before using antibiotics, this could tip the balance. And our experience is that, having got an opportunity to grow, yeast often increases gradually over time, so its symptoms sneak up on you so slowly you may not realize that’s why you are feeling unwell. Some patients have been gradually feeling worse for years before we find that Candida is the cause. So supporting your microbiome is good preventative practice.
Although the microbiome is mainly comprised of bacteria, it also contains some other yeasts. Saccharomyces boulardii, a friendly yeast species, was the first microbe identified to reduce Clostridium difficile-associated diarrhea. And because it isn’t a bacterium, it can be taken with anti-bacterials without being killed off.
We don’t yet know exactly which antibiotics kill off which probiotics, so we can’t give targeted replenishment after antibiotic therapy. But we do know which strains to focus on to avoid diarrhea. We find in practice that people often do better with broad-spectrum probiotics after broad-spectrum antibiotics, which only makes sense!
When you are taking probiotics while on a course of antibiotics, it is best to take the probiotic at least 2 hours after the antibiotic. And while it is preferable to take probiotics on a full stomach, the antibiotics may have to be taken with food. In this case you can either take the probiotics on an empty stomach or have a little snack with them. And, provided that you aren’t taking an antibiotic at bedtime, you can take some probiotics at night, when your digestive system is moving them through your gut more slowly. This will allow more of a chance for the beneficial probiotics to attach to your gut wall, where they can help you.




Comments